Establishing a "Baseline"
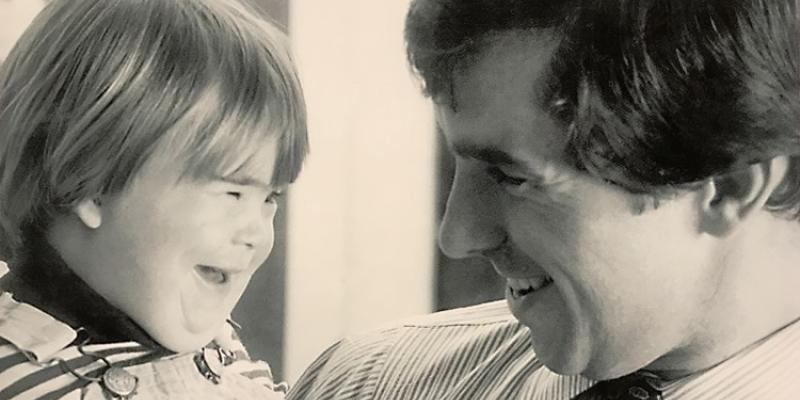
Most adults with Down syndrome will not self-report concerns about memory. Instead, it will take an astute caregiver who knows the individual well to identify early changes or concerns and bring them to the attention of a medical professional. Alzheimer’s disease is suspected when there is a change or a series of changes seen in an individual as compared to their previous level of functioning. Thus, in order to observe change effectively, one must be informed about what the individual was capable of doing at his or her very best. This could be considered the individual’s “baseline.”
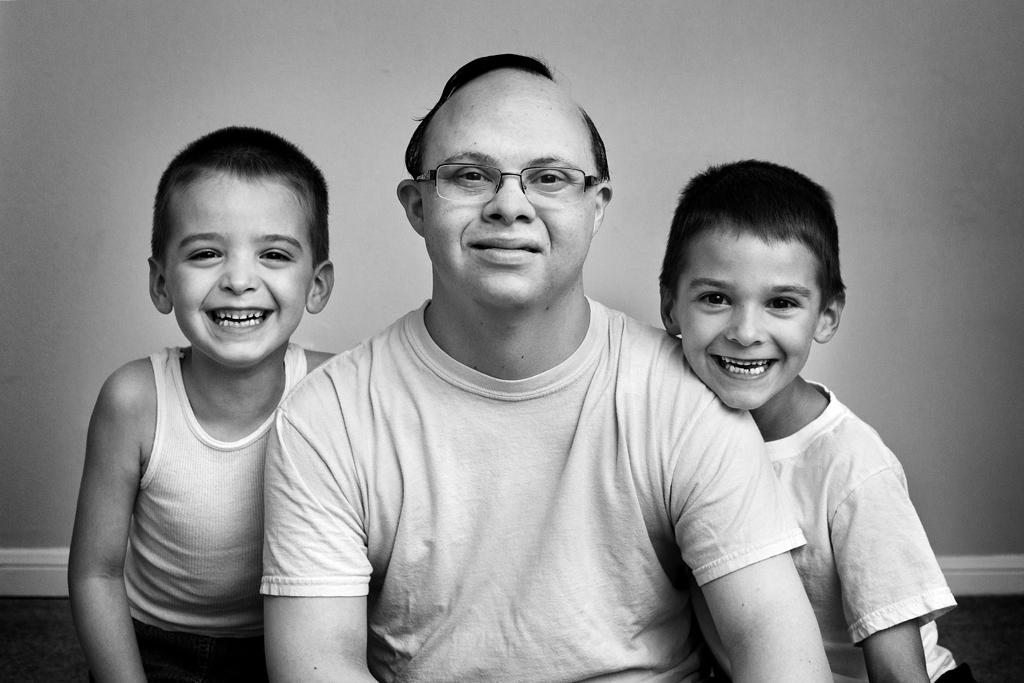
The primary importance of having a good description and understanding of an individual’s baseline is so it can be used as a basis of comparison if changes are observed as the individual grows older. It is extremely helpful to record baseline information throughout adulthood – noting basic self-care skills, personal achievements, academic and employment milestones, talents, skills, and hobbies. A baseline can also be established formally at an office visit with a memory specialist, where these components can be reviewed and memory abilities can be tested.
Formal screening for memory concerns should be a priority throughout mid-to later-adulthood. Alzheimer’s disease is a clinical diagnosis. That means that it requires a doctor to make the diagnosis based on their judgment. There is no single blood test, x-ray, or brain scan that will make or confirm the diagnosis. The diagnosis depends largely on an accurate history detailing progressive loss of memory and daily functioning. It is vitally important that a history be provided by someone (a family member, a longtime caregiver, etc.) who knows the person well. It is important to seek the opinion of a specialist who will take all factors into account to arrive at a diagnosis thoughtfully. It is worth the effort to not rush the diagnosis. Make sure that the assessment has been thorough and that all other possibilities were given careful consideration. Note that many of the common conditions related to aging and Down syndrome outlined in the beginning of this article can be mistaken as dementia if not identified properly (hearing loss, low thyroid function, vision loss, pain, sleep apnea, etc.). If the individual is showing change compared to their baseline memory or functioning, it is important to consult with the primary care doctor to assess for the presence of these other potentially treatable or correctable conditions.
Seeking A Memory Evaluation
Look for a memory specialist (a geriatrician, neurologist, psychiatrist, or neuropsychologist). Ideally, the specialist would have experience assessing individuals with intellectual disabilities. Assessments should be comprehensive and adapted appropriately for each person’s baseline intellectual disability. A thorough assessment should take into account all other potential contributing factors (medical, psychiatric, environmental, social) that could also account for, or contribute to, the reported changes.
After The Diagnosis Is Made
First, make sure that the diagnosis seems accurate. Was it arrived upon in a thoughtful and thorough manner, carefully excluding other possible causes that may explain the changes that were observed and reported?
Next, be proactive in building a support network. The key feature of Alzheimer’s disease is that it is a progressive disorder, meaning it is expected that the individual’s needs are going to increase over time. The support network encompasses the primary care doctor, memory specialist and other related medical specialists, caregivers, day program or workshop staff, state or agency support staff, other family, friends, etc.
Learn About Dementia
This article aims to provide a basic introduction to this topic, but one should seek out other resources to learn more and to get support. Some resources are provided at the end of this page.