Sleep apnea is a problem with breathing during sleep that can lead to decreased oxygen levels and frequent arousals (brief wake ups you typically don't remember). There are two main types of sleep apnea: obstructive sleep apnea (OSA) and central sleep apnea (CSA). OSA is the most common and occurs when the airway is physically blocked. CSA is much less common and occurs when the brain does not send the correct signals to the muscles that control breathing.

Individuals with Down syndrome are much more likely to have OSA than individuals without Down syndrome. Studies have suggested 53-76% of children and more than 80% of adults with Down syndrome have OSA, compared to about 2-6% of children and 10% of adults without Down syndrome. This may be due to factors that tend to occur at higher rates in individuals with Down syndrome such as:
• facial structure differences.
• narrow airway in the nose and throat.
• low muscle tone.
• poor coordination of airway movements.
• obesity.
Children with Down syndrome may have enlarged adenoids, tonsils, and tongues obstructing the already narrowed airway. Some individuals with Down syndrome experience more frequent sinus and upper respiratory infections. This causes congestion which can worsen obstruction. Gastroesophageal reflux (GERD) is also associated with OSA, and the relationship between the two is being researched (Kim et al., 2017).
Potential Impacts
Untreated OSA in individuals with Down syndrome can lead to unwanted behaviors and decreased language, memory, and emotional control.

If the individual is a child, they might:
- Have tantrums.
- Be less willing to use words to communicate.
- Have trouble learning new skills.
An adult may:
- Refuse to participate in normal activities.
- Be less willing to engage in conversations.
- Forget parts of their usual routine.
- Have difficulty following directions.
Sleep apnea also increases the risk of:
- Heart disease.
- Arrhythmias (irregular heart rate).
- Congestive heart failure.
- Pulmonary hypertension (high blood pressure in the lungs).
- Stroke.
These potential impacts of untreated OSA highlight the importance of early identification and treatment (Shott et al., 2006).
Signs and Symptoms

Symptoms of sleep abnormalities may include:
• restless sleep.
• snoring.
• gasping noises.
• heavy breathing.
• apneic pauses (a pause in breathing).
• frequent waking during the night.
• trouble getting out of bed.
• daytime sleepiness.
• excessive napping.
• unusual sleep positions (such as sitting upright or keeping the head and neck tilted backward).
Some children with Down syndrome and OSA may not have any apparent symptoms. A sleep study by age 4 years old is recommended for all children with Down syndrome due to the high risk of OSA. Caregivers should alert a doctor to any change in sleep, mood, behavior, or ability to concentrate.
Sleep Studies
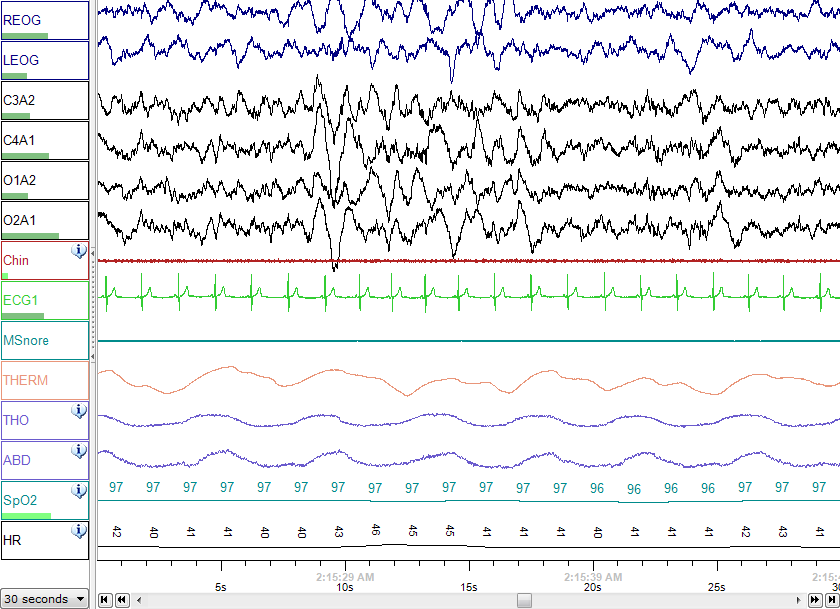
(pictured left: Polysomnography (sleep study) record of sleep) In 2011, the American Academy of Pediatrics recommended all children with Down syndrome have a polysomnography (PSG), or a sleep study, by 4 years of age. The PSG consists of a night of observed sleep during which professionals measure brain waves, the oxygen level in the blood, heart rate, breathing, and eye and leg movements. Children who are unable to have a PSG due to lack of access or inability to tolerate the conditions might have a home sleep study or home pulse oximetry.
Studies have shown parents are often unable to correctly predict whether their child with Down syndrome has a sleep-breathing disorder. This is why it is so important to have testing done by professionals (Friedman et al., 2018; Shott et al., 2006). However, it can still be beneficial for caregivers to know what signs and symptoms to watch for.
Treatments
Tonsil and Adenoid Removal
There are treatment options available for OSA. Some people with Down syndrome have relatively smaller jawbones, cheekbones, and eye sockets and narrow nasal passages. This can lead to airway obstruction when tonsils and adenoids are even slightly enlarged. Because of this, the most common treatment in children is adenotonsillectomy (surgical removal of tonsils and adenoids). A sleep study should be repeated after this surgery to determine whether the OSA was resolved.
Unfortunately, adenotonsillectomy does not always cure sleep apnea. Up to half of children with Down syndrome experience OSA that continues even after surgery to remove tonsils and adenoids, known as “residual” OSA, though most children will see a decrease in OSA severity, even if it doesn't resolve completely. MRI studies have shown a combination of relatively large tongues, glossoptosis (backward movement of the tongue during sleep), and tonsil and adenoid regrowth are the most common causes of residual obstruction. To determine the site(s) of residual airway obstruction, your doctor might perform a nasopharyngoscopy and laryngoscopy examination. A flexible lighted camera is inserted through the nose or mouth to examine the area behind the nose, the back of the tongue, and the throat. This can rule out regrowth of tonsils or adenoids and glossoptosis.
CPAP/BiPAP Use
Continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP) therapy is often used as a secondary treatment after surgery.
CPAP: A machine that delivers a steady stream of air through a flexible tube to a mask sealed around a person’s nose and mouth. The airstream pushes against any obstructions, maintaining an open airway for breathing. CPAP machines are primarily used to treat OSA.
BiPAP: A machine that delivers a stream of air at two pressures: an inhale pressure and an exhale pressure. It is used for individuals who cannot tolerate CPAP machines and to treat central sleep apnea.
CPAP and BiPAP machines are typically life-long treatments. Although many individuals with Down syndrome adjust to using the CPAP during sleep, some are unable to tolerate wearing the facial mask and require alternative treatments.
Hypoglossal Nerve Stimulation
Hypoglossal nerve stimulation (an implanted medical device that electrically stimulates tongue movement with breathing) is a relatively new treatment researchers are hopeful about. This was studied specifically in adolescents with Down syndrome and found to improve OSA severity by 53% (Yu et al., 2022) and was FDA-approved for use in people with Down syndrome as young as 10 years old in 2023.
Other treatments:
• A high-flow nasal cannula used at night (oxygen provided through the nose in a tube): This may be effective but has limited evidence and is often difficult to obtain.
• Anti-inflammatory medications: These may have limited effectiveness in children with Down syndrome. Two small studies did not show any improvement in OSA severity in children with Down syndrome with these treatments (Yu et al., 2020).
• Myofunctional therapy (exercise-based therapy for the muscles of the mouth, tongue, and face): One small study of one week of myofunctional therapy did not show benefit for OSA in children with Down syndrome (von Lukowicz et al., 2019). It is possible that long-term treatment may be needed to see a benefit.
• Dental devices worn at night that push the lower jaw forward
• For individuals who are medically overweight, getting to a healthy weight can improve symptoms.
• Atomoxetine and Oxybutynin: This medication combination has shown an improvement in OSA severity of about 50% in children with Down syndrome (Combs et al., 2023).
More research is needed on these treatment options for individuals with Down syndrome. All options should be discussed with a doctor to determine which is best for you or your loved one.
Thank you to Daniel Combs, MD, Assistant Professor of Pediatrics and Medicine at the University of Arizona, who provided updates to this webpage.
Additional Resources
External Resources
- American Sleep Apnea Association
www.sleepapnea.org
Promotes awareness of sleep apnea, works for continuing improvements in treatments for this serious disease, and advocates for the interests of sleep apnea patients - American Sleep Disorders Association
www.sleepassociation.org
A national organization focused on improving public awareness about sleep disorders and sleep health, promoting sleep medicine research, and providing a portal for communication between patients, physicians/healthcare professionals, corporations, and scientists - National Sleep Foundation
www.sleepfoundation.org
Dedicated to improving sleep health and safety through education, public awareness, and advocacy.
Citations
Combs D, Edgin J, Hsu C-H, et al. The combination of atomoxetine and oxybutynin for the treatment of obstructive sleep apnea in children with Down syndrome. J Clin Sleep Med. 2023;19(12):2065-2073.
von Lukowicz, M., Herzog, N., Ruthardt, S., Quante, M., Iven, G., & Poets, C. F. (2019). Effect of a 1-week intense myofunctional training on obstructive sleep apnea in children with Down syndrome. Archives of disease in childhood, 104(3), 275–279. https://doi.org/10.1136/archdischild-2018-315064
Yu PK, Stenerson M, Ishman SL, et al. Evaluation of Upper Airway Stimulation for Adolescents With Down Syndrome and Obstructive Sleep Apnea. JAMA Otolaryngol Head Neck Surg. 2022;148(6):522–528. doi:10.1001/jamaoto.2022.0455
Yu W, Sarber KM, Howard JJM, et al. Children with Down syndrome and mild OSA: treatment with medication versus observation. J Clin Sleep Med. 2020;16(6):899–906.







