Understanding behavior is crucial for creating inclusive and supportive environments for individuals with Down syndrome. Humans engage in behaviors every single day, yet it can still be difficult to understand and interpret why a behavior is occurring. By gaining deeper insight into why behavior occurs, we can promote overall wellbeing, improve social interactions, and provide resources to help individuals thrive.
Definitions of commonly used words and phrases
Behavior
What a person does that can be observed (e.g., seen or heard) and measured. This includes actions such as speaking, smiling, walking, pointing, or playing a video game. Thoughts, emotions, and feelings are not behaviors (although they are still important!).
Behavior change
Differences in a person’s observable actions, as compared to their previous or typical behavior. This can include desired behaviors, such as successful toilet training, but can also include behaviors that present challenges or barriers to the person’s quality of life. Behaviors that are not typical but not necessarily undesired can be neutral or positive changes in how a person acts.
Behavior challenge
Observable actions that create a barrier to an individual's quality of life, impede the occurrence of desired behaviors, and/or jeopardize the health and safety of themselves or others. Behavior challenges can also be the same behavior that has been observed as the behavior change.
Behavior analysis
A general term used to encompass various evidenced-based approaches to understanding how a person’s environment impacts their behavior. Behavior analysis includes ways to teach new skills, maintain/increase desired behavior, and reduce behavior challenges.
Function of Behavior
In applied behavior analysis, function is a term used to describe the reason any behavior occurs. There are four functions (or reasons) behavior analysts use to explain behavior: access to items and/or activities, access to attention, escape/avoidance, and sensory responses (e.g., pain attenuation, sensory reinforcing activities).
Understanding Behavior
When a person thinks of behavior, they often think of actions that are problematic, maladaptive, or atypical. However, behavior is everything we do and say. It includes not only negative actions, but positive and neutral actions as well such as brushing teeth, saying “hello”, smiling, tying shoes, and talking with friends. It is important to recognize and address behaviors that lead to challenges at home, school, or work, cause stress to a caregiver, decrease quality of life, or jeopardize the health and safety of the individual or those around them.
Behavior Across the Lifespan
Behavioral challenges seen in individuals with Down syndrome have the potential to be present in unique ways. Behavior challenges are usually noticed during or after a behavior change. A behavior change can be caused by many factors. Medical, social, environmental, and psychological shifts can all lead to behavior changes. The behavioral challenges seen in children with Down syndrome are usually not particularly different from those seen in typically developing children. However, they may occur at different developmental times, look different in their presentation, and require more individualized strategies. Additionally, some individuals have difficulty with the transition into adulthood as they face the loss of social networks, departure of siblings, death of loved ones, changes in housing, and the challenge of obtaining meaningful work or activities.
Other complexities, such as unique communication skills, can also impact behavior. It is necessary to be familiar with the individual’s preferred receptive and expressive language method and style because many behaviors are related to communication.
- Expressive communication is how a person uses their own words, sounds, gestures, or body positioning to convey their wants and needs.
- Receptive communication is how a person understands communication from another person in the form of words, sounds, gestures, social, and environmental cues.
For example, how a person expresses pain may not include clear verbal statements, such as, “My stomach hurts.” Expressions of pain can include gestures, general statements of not feeling well, refusal to eat, atypical behaviors, or other changes. A common misconception is that a person’s expressive communication skills are always the same as their receptive skills, which can lead to miscommunication and misunderstandings. For example, a person may easily understand all verbal communication but have difficulty speaking and enunciating clearly.
A special note for aging individuals with Down syndrome is the increased frequency of early onset Alzheimer’s disease. Alzheimer’s disease has its own characteristics and symptoms that can impact not only a person’s behavior but also their overall functioning. To learn more about Alzheimer’s disease in individuals with Down syndrome, please check out our free guidebook, Alzheimer’s Disease and Down Syndrome: A Practical Guidebook for Caregivers.
Why Does Behavior Happen?
A common approach to understanding behavior is through the lens of behavior analysis. You do not need to be a behavior analyst to understand behavior, but the concepts may be helpful when trying to determine the cause of a certain behavior. It is important to note that determining the cause of behavior takes time. Be patient with yourself and your loved one as you work through this process.
Once it is understood why a behavior is occurring, finding successful interventions becomes easier. For behavior analysts, all behaviors are related to at least one (but commonly two or more) of the following functions (reasons):
- Access to attention
- Access to items/activities
- Escape/avoidance
- Sensory response/pain response
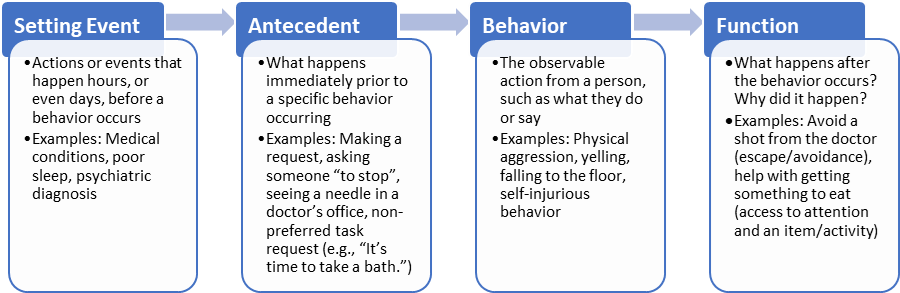
First, we need to start by gathering more information about the patterns and characteristics of the person’s behavior change to better understand why the behavior is occurring. By understanding the different parts of the behavior and the order in which they occur, we can develop specific strategies to help prevent or manage the occurrence of behaviors. For this, looking at behavior as a model can be helpful.
Medical Conditions and Behavior
A vital step in evaluating an individual with Down syndrome who has a behavior concern, particularly if it is new or appeared suddenly, is to rule out medical conditions that could be causing the behavior. Medical professionals with a working knowledge of the person, along with caregivers providing medically relevant history of the symptoms, are best able to guide medical treatment. Below is a non-exhaustive list of questions that can be reviewed with your physician to decide if there may be a medical reason for the behavior concern:
- Has the behavior had a sudden onset? Has the behavior always occurred, but the frequency or intensity changed suddenly? Has a “typical” behavior suddenly stopped?
- Is the person holding, pushing, squeezing, hitting, pointing to, avoiding, protecting, or otherwise focused on a specific area of the body?
- Have they shown changes in their sleep patterns? Excessive sleep? Awake at night? Only sleeping for short periods? Difficulty falling asleep vs difficulty staying asleep?
- Are they eating differently? Changes in quantity or frequency? Hard vs soft, hot vs cold foods? Have food preferences changed?
- Changes in urinary or bowel regularity?
- Was there a recent medication change?
- Was there a recent medical procedure or appointment (e.g., dental visits, accident/injury, doctor visit)
- Do they have chronic medical conditions? Diabetes, GERD, constipation, diarrhea, etc.
- Have there been recent changes to social systems (e.g., home, work, school, family) or abrupt changes in mood or feelings?
- Is there a change in cognitive status, such as confusion, memory loss, mood changes? The following are areas that can potentially impact cognitive status:
- Environmental – Changes in work, school, routine, or schedule
- Social – Grief issues, changes in family dynamics, stress management
- Medical – Rapid/sudden changes in mood, undiagnosed/untreated medical issues (short-term vs long-term), changes in medications or medical treatments.
- Has the specific behavior occurred before? What was the cause and resolution to the previous occurrence of the behavior?
Psychotropic Medications and Behavior
A psychotropic medication is any drug affecting a person’s mood, behavior, thoughts, or perception of their environment. These medications have become increasingly common to address atypical behavior in individuals with any form of intellectual disability but should be used with caution and understanding. The use of psychotropic medications is most effective when combined with a comprehensive, interdisciplinary plan of care addressing all the needs of a person.
If taking psychotropic medications, it is essential for the individual, caregivers, and any person providing support to understand what the prescribed medication is for and how it can impact the individual taking it. It is also important to know how other medications interact with psychotropic medications. Be sure to share all medications both past and current with the prescriber. This is essential information for medical professionals and caregivers alike, as it is not uncommon for medications to have multiple uses. For example, there is a medication that can be used to treat high blood pressure as well as hyperactivity. A few common questions you might ask a prescribing medical professional are:
- Why is this medication being used? Does it have other uses as well?
- How long will it take the medication to begin working?
- What are the potential side effects from the medication? What is the likelihood of experiencing these side effects? What should I do if I experience them?
- How will I take the medication: what time(s), with or without food, administration route (e.g., oral, topical, injection, etc.), for how long?
- Will it impact other medications I am taking?
Evaluation by a qualified medical professional is a vital component of the management of all healthcare needs, including behavior concerns, in children and adults with Down syndrome. The NDSS Caregiving and Down Syndrome: A Companion Guidebook to Aging and Down Syndrome: A Practical Guidebook for Caregivers is an available resource to provide insight into medications and Down syndrome.
Accessing behavior analytic services can vary greatly depending on many factors such as age, setting, and insurance accessibility. When looking for behavior analytic services, age can be a large determinant of “where to start.” If the person who may need behavior analytic services is an infant before the age of 5, Early Intervention programs, usually directed by state health agencies, are recommended as a first resource. If the person is school-age, contacting your local school district would be a good first place to start for resources. If the person is an adult, case management or social workers would be a front-line resource to assist. A sample of resources for understanding behavior analysis as an intervention can be found under External Resources below.
The information provided herein is for informational purposes only. NDSS is not a health care provider, and this information should not be construed as medical advice or a substitute for it. Please consult with your or your family member’s health care provider(s) to determine your/their personal health care needs (if any).
NDSS thanks Ley Linder for his significant contributions to this page.
Ley Linder, MA, M. Ed., BCBA
Intensive Behavior Interventionist
President and CEO of Crescent Behavioral Services
Internal Resources
- Alzheimer’s disease guidebook
- Caregiving guidebook
- Regression webpage